The New England Journal of Medicine recently published a paper showing the highest spatial-resolution estimates of malaria mortality in Africa to date. Malaria No More spoke to one of the study’s authors, Dr. Simon Hay of the Institute for Health Metrics and Evaluation at the University of Washington in Seattle, about the significance of the research.
Why did you undertake this study?
We wanted to highlight the potential for high-resolution maps to help us better understand the epidemiology of malaria as well as the contribution of recent control efforts. We believe the information could help inform future malaria control efforts.
In your opinion, what are the most important findings?
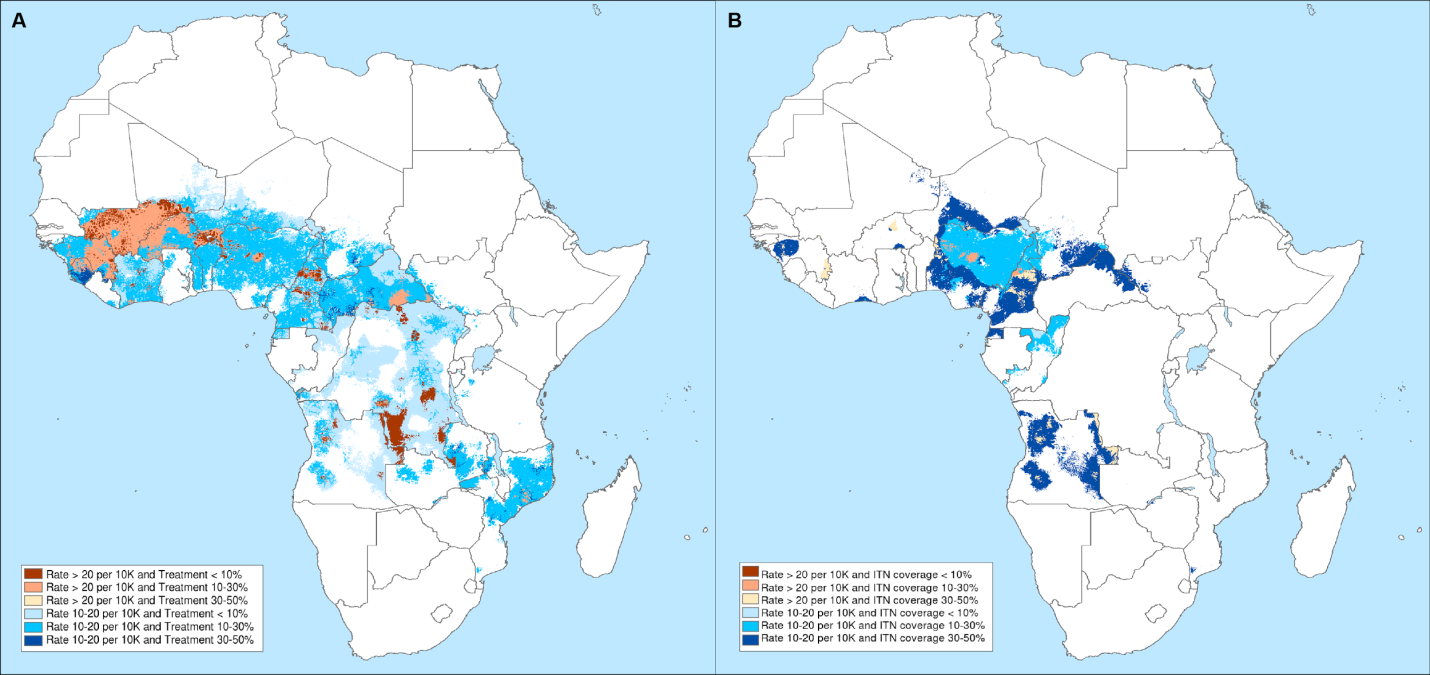
There was an overall decrease of 57 percent in the rate of death from malaria across sub-Saharan Africa. We identified high-risk areas that have low coverage of both preventive and treatment interventions, which highlights the potential for more targeted malaria control efforts.


Photo courtesy of The Institute for Health Metrics and Evaluation (IHME).
Your numbers on malaria mortality differ from those presented by the World Health Organization (WHO). Why is there a discrepancy in the annual number of malaria deaths in Africa between this report and WHO’s World Malaria Report?
It is important to note first that our numbers and WHO’s numbers have overlapping uncertainty intervals. The differences are due to the way estimates are generated. We use a new method that builds on the previous work of the Malaria Atlas Project in estimating malaria prevalence and incidence, and then combines that with estimates of malaria mortality from the Global Burden of Disease study.
What makes this study so revolutionary?
No other study has estimated malaria mortality across sub-Saharan Africa on a 5 km by 5 km grid. This study brings malaria mortality to a novel spatial resolution. Moreover, it combines two rigorous and well-respected methodological approaches to answer a timely question: Where does malaria still cause death, and how might that burden be alleviated?
How do you think this will impact programmatic work on the ground?
Understanding the distribution of malaria deaths on a small geographic scale over time will allow us to measure the effects of malaria control programs, which has huge implications for public health policy. These maps also have the potential to help guide more efficient and effective malaria control strategies that take into account the spatial distribution of malaria burden. Our study also highlights the importance of strategies to prevent both drug and insecticide resistance.
These maps show us where different types of interventions have been implemented and what kind of impact they’ve had. They show us which areas need more attention and where we need more information. Combining these threads through space and over time can result in powerful interventions.

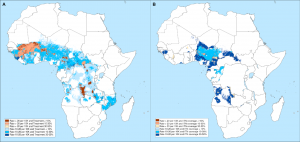
Photo courtesy of The Institute for Health Metrics and Evaluation (IHME).
What gaps did this study identify? Where do we still need more information?
The major gap is the relative lack of timely, high-quality data on malaria mortality across all countries in sub-Saharan Africa.
What implications does this study have for the way we look at global health trends?
This study shows that understanding mortality and epidemiologic trends at a fine spatial resolution allows for new perspectives. Through our geographic approach, we can provide results in a traditional manner (e.g. number of deaths in a country) while simultaneously being able to look at internal variation at a fine scale.